If you’ve never had gallstones, you’ve probably never thought about your gallbladder. However, if you have had gallstones, chances are good that you have had your gallbladder removed. Either situation has its own inherent issues, and one thing that healthcare providers rarely tell gallbladder patients is that surgery will forever impair their digestion and may make losing weight very, very difficult.
The gallbladder is a small, pear-shaped organ under your liver that concentrates and stores the bile that your liver produces to aid fat digestion. Most people don’t give it a second thought until it starts to trouble them, and unfortunately, for many years, the medical establishment didn’t realize the full importance of healthy gallbladder function. They felt its removal had few, if any consequences. I am of the opinion that we were not designed with unnecessary parts, and the gallbladder is no exception. In fact, science is just beginning to understand the true importance of healthy gallbladder function and the detrimental consequences of its dysfunction or removal.
Each day, your liver produces ~27-34 ounces of greenish-brownish-yellow bile, which is concentrated anywhere from 5-18 times, and then 1-3 oz is stored in the gallbladder awaiting your next meal. When you consume foods containing dietary fats, your gallbladder is triggered to release this concentrated bile into the first part of the small intestine, the duodenum, where it acts as an emulsifier to break down those fats and aids in the absorption of the fat soluble vitamins, A,D,E, & K, and any essential fatty acids. If you have ever vomited until a bitter, yellow substance came up — that was bile, and while you may not have thought so at the time – bile itself is an amazing substance. Comprised of bile acids, bile salts, cholesterol, phospholipids, pigments, water, electrolytes, and amino acids, bile is a bitter, acidic substance that breaks down fats into components that the body can use. Healthy fat absorption is crucial to our health. In fact, we were designed to eat fats rich in healthy fats. Our brains, our hormones, and even our very cell walls are dependent on a steady and healthy supply of fat soluble vitamins and essential fatty acids.1 Vitamin A is an important antioxidant that plays a crucial role in cell division, cell differentiation, reproduction, immune function, growth, and vision. Vitamin D is a prohormone which not only regulates calcium metabolism, but is essential for the functioning of the nervous system, for bone health, for muscle strength, for immune function, regulating blood pressure, hormone production and for cell differentiation. Vitamin E is a blanket term for eight different nutrients (4 types of tocopherols and 4 types of tocotrienols) that have string antioxidant properties and also play a role in immune function, healing, repair, and cardiovascular functioning. Vitamin K is a nutrient that scientists are just starting to devote research time to. It is known to play a key role in bone health, blood clotting, and heart disease, but studies are showing that it may have many more far-reaching effects. Essential fatty acids (EFA’s), such as omega-3 fatty acids, are ESSENTIAL to human functioning. Long recognized for its powerful anti-inflammatory benefits, EFA’s are required to make the cell walls of every cell in your body and they play a key role in immune functioning, musculoskeletal health, cognitive function, and heart disease. Considering the overwhelming importance of fatty acids and fat soluble nutrients to general health, it makes no sense to willingly cut out gallbladders with no plan of action to compensate for the deficit caused by its dysfunction or removal. Whether you have a gallbladder that isn’t doing its job or you have already lost yours – there is a solution.
So, how does all of this apply to lack of weight loss — or worse, weight gain?
In simplistic terms, the body is a finely tuned organism. We need 17 nutrients in specific quantities just to make adequate levels of stomach acid and other digestive substances. When gallbladders dysfunction, two things can happen: First, the bile gets too thick and stagnant, which creates an ideal situation for gallstone formation. Second, when gallstones impair or block the emptying of the gallbladder, fat digestion decreases dramatically, which in turn, puts your body into starvation mode. The body requires the absorption of those fat soluble vitamins and essential fatty acids, but it recognizes it is in a chronically deficient state – so it hangs on to the fat it has (which unfortunately may be that stomach pooch) for dear life. You in turn want to lose that stored fat, and may erroneously take on a low-fat diet at the advice of your healthcare provider, which only makes the matter worse.
Causes/Risk of Gallbladder Dysfunction
- hypochlorhydria (low stomach acid)
- low fat diets
- high fat diets
- food allergies and sensitivities
- gluten intolerance
- being overweight
- dieting, rapid weight loss
- pregnancy
- sedentary lifestyle
- birth control pills or hormone replacement therapy
- heartburn
- use of antacids and Proton Pump Inhibitors (PPIs)
- 40+ years of age
- females are at greater risk in the United States (in other countries, males can be at higher risk – it is thought that alcohol consumption plays a causative factor there). Women that have birthed children also have a greater risk of developing gallbladder dysfunction
- alcohol use (the more you drink, the greater your risk)
- bariatric surgery
- ethnicity (more prevalent in Native American populations and Hispanics)
- family history of gallbladder issues
- extreme diets which eliminate any key food group
- elevated cholesterol, especially high triglycerides or LDL
- consumption of statin medication or immunosuppressive medication
- medical conditions including hypothyroidism, diabetes, insulin resistance, inflammatory bowel disease, PCOS, hemolytic anemia, etc.
- western diets, diets high in refined carbohydrates and sugars
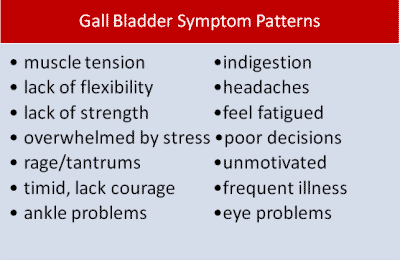
That’s a long list of risk factors – it’s a miracle that anyone has a normal functioning gallbladder given our Standard American Diet (SAD) and reliance on fried and processed foods. In fact, gallbladder dysfunction is so common that clinicians refer to it as the 4-F syndrome: Female, Fat, Forty+, Flatulent. However, most people with gallbladder dysfunction are asymptomatic. Studies estimate that anywhere from 67-80% of people with gallstones have no symptoms. That said, many people discount gallbladder symptoms as being related to poor digestion or other factors. Everyone with gallstones started off with thick or stagnant bile. You have to have one to lead to the other. The pattern of symptoms associated with gallbladder dysfunction is so varied that many people without digestive pain may not associate their muscle pain, dry skin, poor wound healing, dry (or shedding) hair, headaches, heel calluses, or inability to lose weight despite doing everything right with a gallbladder that is not operating at par.
Symptoms of gallbladder dysfunction: Most commonly: pain or discomfort after eating. This can include gas, bloating, belching, heartburn, nausea, queasiness abdominal discomfort, extreme fatigue, pain under the ribs, particularly on the right side, or shoulder pain. Additional symptoms include headaches over the right eye, constipation or diarrhea, light colored or ‘floating’ stools, dark urine, offensive body odor or breath. People with gallbladder dysfunction tend to have bowel extremes — they experience diarrhea (up to 10 bowel movements per day) or constipation (often having days between bowel movements) and rarely have normal bathroom habits.
Have you had your gallbladder removed? You are not alone. Over half a million gallbladders are removed every year in the US. It is one of the most commonly performed surgical procedures. Symptoms of postcholecystectomy syndrome (PCS): gas, bloating, belching, heartburn, nausea, queasiness abdominal discomfort, extreme fatigue, pain under the ribs, particularly on the right side, or shoulder pain. The need to run to the bathroom immediately after eating is fairly common. Additional symptoms include headaches over the right eye, constipation or diarrhea. Notice the symptoms are almost exactly the same for people with NO gallbladder as for those with a dysfunctional one? Researchers estimate that at least 40% of people who have had gallbladder removal continue to experience significant abdominal pain.2 It is estimated that 5-40% of people who have had a cholecystectomy experience long term symptoms from it . 3 One British study looking at the after-effects of gallbladder surgery found that 87% of men and 68% of women experienced weight gain after cholecystectomy and urged physicians to caution patients about this ‘side-effect.4 I can easily say that in my 12 years of practice, I have NEVER had a gallbladder patient tell me that they were informed of the likelihood of weight gain prior to their surgery!
Where Weight Gain & Weight Loss Issues Come into Play
Having a dysfunctioning gallbladder or having no gallbladder are both associated not only with difficulty losing weight, but with weight gain. Anecdotal reports are abound of women having few issues maintaining their healthy weight until they had gallbladder removal surgery. On a functional level, we know that nutritional deficiencies are associated with difficulty losing weight, and by drastically impairing fat digestion through having stagnant bile or by surgical removal of the gallbladder – we create the foundation for broad-spectrum health disorders. Our bodies are designed to maintain an equilibrium, or steady state. It craves balance. So when we have gross nutritional deficiencies, our bodies inherently want to hang on to its stores of fat and nutrients. It doesn’t want to exacerbate its deficient status by losing more of anything – and that includes your love handles.
So, what can you do about it?
1) First and foremost, you need to concentrate on eliminating the nutritional deficiencies. This is imperative if you want to get your body out of starvation mode. I suggest that you take a high-quality, highly absorbable multivitamin. Look for a high potency multivitamin that contains more than the 100% RDA amounts. Those amounts were designed to keep a person out of gross deficiency status, they are not amounts your body needs for optimal functioning.
2) The second thing I recommend is supplementing with pancrealipase and organic beet extract. I carry two different formulas – one for people with gallbladders who need to thin their bile so their digestion works better and another for people who no longer have a gallbladder and who need to add ox bile extract in addition to the pancrealipase and organic beet extract so they can start breaking down those dietary fats , get themselves out of a deficient status, and start losing weight. Either formula can be ordered directly from me (message me through facebook), or through the manufacturer. These supplements are only sold through licensed healthcare providers, and I am prohibited from publishing prices publicly, but if you visit my facebook group https://www.facebook.com/groups/weightlossresources/ and check the FILES section. I have included complete ordering information along with a discount code for my clients.
3) Limit your intake of refined carbohydrates. Not only are these typically ’empty’ calories, but they rob you of minerals like magnesium and chromium, and your b-vitamins. They also induce insulin spikes which further stress your liver and gallbladder.
4) Increase your magnesium intake. Whether you take oral magnesium preparations, or you use epsom salt baths – magnesium has been shown to prevent gallstone formation. It is also required for making appropriate levels of stomach acid.
5) Increase your intake of taurine-rich foods. Taurine is one of the major amino acids found in bile. Healthy digestion depends on getting adequate supplies of taurine. Meat, eggs, seafood, certain dairy products, and brewers years are all good sources of dietary taurine.
6) Eat healthy fats! Your body needs fat in order to lose fat. If fat digestion troubles you, start slowly with small amounts of unrefined organic coconut oil and slowly add other healthy oils into your diet. Let your body accommodate to them. Healthy fats include grass-fed butter (which is a source of vitamins A,D,E,K, as well as selenium, and CLA), ghee, lard, egg yolks, organ meat, palm oil, olive oil, most nut oils, etc. Bad fats include corn oil, soy oil, canola oil, sunflower oil, safflower oil, cottonseed oil, margarine, and anything listed as ‘hydrogenated’. These refined oils are a source of omega-6 fatty acids which not only contribute to obesity but cause inflammation within the body, and that includes liver and gallbladder inflammation.
In short, having gallbladder problems or no gallbladder whatsoever need not cause you issues. There are simple solutions that allow your body to work the way it was intended to. You can get the weight off and avoid the bizarre food cravings that come along with those nutrient deficiencies. You can feel normal after meals. You can have normal bowel movements, and you can get rid of the fatigue that overwhelms you. If you combine healthy food choices along with the simple supplements I suggest, you will see results. If you are able to combine the two with lifestyle improvements you will see results that much faster. I sincerely wish that more medical providers educated their patients on the detriments of gallbladder surgery before they submitted to it, so they could take preemptive action, however, in the words of Mick Jagger, “you can’t always get what you want, but if you try sometime, you just might end up with what you need”. So, in closing, I hope this information is what you need. Please visit me on facebook at Weight Loss Resources with Dr. Miranda. If abdominal pain persists, you may have a problem caused by something other than the gallbladder. Other possible causes of abdominal pain include irritable bowel syndrome, inflammatory bowel disease, stomach ulcers, or pancreatitis. Please seek the advice of your licensed healthcare provider to rule out serious health conditions.
♥♥♥Other posts of mine that you may find helpful (click on any of the blue text below to open) :
-
What happens to your body after gallbladder surgery
-
When good gallbladders go bad
-
Weight Loss that Really Works
-
Are these 4 hormones making you fat?
1) http://www.webmd.com/digestive-disorders/picture-of-the-gallbladder
2) Hearing, L Thomas, K Heaton, L Hunt
Post-cholecystectomy diarrhoea: a running commentary Copyright © 1999 BMJ Publishing Group Ltd & British Society of Gastroenterology.
3) http://www.webmd.com/digestive-disorders/tc/postcholecystectomy-syndrome-topic-overview
4) Weight gain after cholecystectomy. BMJ 1984; 289 doi: http://dx.doi.org/10.1136/bmj.289.6455.1350 (Published 17 November 1984)Cite this as: BMJ 1984;289:1350
Other sources:
1. Bates T; Ebbs SR; Harrison M; A’Hern RP.Influence of cholecystectomy on symptoms.
Br J Surg. 78(8):964-7, 1991 Aug.
2. E Ros, D Zambon . Postcholecystectomy symptoms. A prospective study of gall stone patients before and two years after surgery. 1987 BMJ Publishing Group Ltd & British Society of Gastroenterology
3. CAROLE MACARON, MD,MOHAMMED A. QADEER, MD, MPH, JOHN J. VARGO, MD, MPH, Cleveland Clinic Journal of Medicine March 2011 vol. 78 3 171-178, Recurrent abdominal pain after laparoscopic cholecystectomy
-
http://www.principlesforparents.com/gall-bladder-energy.html -(graphic)


Another great Blog! The things we learn from you! Keep up the great job!
Thank you Miranda this is a great blog.
I watch what I eat (most of the time LOL) I walk a lot at work or farm work..
I have lost weight in doing that but it was getting to a point where would not budge..started the products you recommended for me and already notice a weight shift.
I would like to thank you for all your hard work you put in for the benefit for others..
Anne
Thank you so much for this article! I had my gallbladder removed last year and have been putting on weight like crazy. It’s making me go insane, especially because I feel hungry all the time. I am definitely interested in (natural) supplements to help me!
This is a very good article. You really have to find your own answers because the doctors don’t tell you everything. Good job
Just came across your article, thanks so much for the info! I had my gallbladder out at 27–I’m 55 now. It was the worst decision to make but there was no Internet to help me understand the issue, and I was in so much pain. I’ve gained an enormous amount of weight since then. Luckily I’ve learned about keto and so far have dropped 45pds. The worst though, has been the hormone deficit all these years, along with a bad diet, which led to years of low level thyroid function and adrenal insufficiency. (I am on so many hormone replacement meds!) I finally had my pregnenolone tested and it was extremely low. Raising it is helping. Can’t help thinking that being without a gallbladder played into this misery and cut short what should have been an active, full life. I wish this headache on no one! Having read your article, I will be more faithful in taking my Ox Bile, etc., to get healthy and get the weight off!;-)
Iam going to have surgery on Tuesday.If there is a way to stop the pain and not under go surgery then help me.
My symptoms right now are legs ache, side hurting.sometime pain over right eye. Do I have to have surgery and can gall bladder rupture. I had a ultrasound done and they didn’t see any of them but they did see liquid. I’m worry.
Thank you so much for this article! I gained so much weight when my gallbladder started acting up and even more once it was removed. I will definitely be purchasing the recommended supplements and will visit your Facebook group page. Other than surgery recovery I’m also juggling untreated hypothyroidism and gastritis, do you have any general advice for that? Again, thanks so much for this helpful article.
I get my gallbladder out on Tuesday and this helped a lot and I hope to do some of the things you mentioned to help me lose weight.. Thanks so much!!
I had my gallbladder removed in Jan. of 15, and have been putting on weight in my stomach every since. My weight had been the same all my adult life until they removed my gall bladder. I had a stone shoot out and lodge into my pancreas which caused severe pain under my right breast. I thought I was having a heart attack. It took them a couple of days to after a scan and a MRI to see if the stone was still in my pancreas, then since my bladder had stones, they decided to take it out. Nothing was ever said about the side effects it would have. Now I am fighting this weight gain. Just last week I told my primary doctor I was worried about my weight, and he checked my thyroid which was normal. I have been walking and cutting back on my eating, but cannot lose weight. My husband is in the same shape as I for he had gained weight, but no energy to do much exercise. I am thrilled to read this article and hopefully I can start doing something about it now. Thanks so much.
Thank you for your kind words. There is a lot that you can do, and supplementation certainly can help. You can order the supplements I most frequently recommend directly from the tab on the blog too for your convenience. If you have not joined my facebook group – Weight Loss Resources with Dr. Miranda, please do so. There is a lot of wonderful information there to get you started!
Thank you so much for posting this article! I had my gallbladder out 8 years ago when I was 25 and luckily I didn’t start feeling the side effects discussed in your article until about 3-4 years ago. Then it all happened fairly quickly: skin discoloration, acne, weight gain all around my stomach, fatigue, but the most frustrating part is the brain fog/memory loss. I hate that I can’t quickly recall things like I used to, or when I honestly can’t think of a simple word during a conversation or meeting. Luckily I found a wonderful naturopath last month who gave the same advice of supplementation. Can you tell me how long you think it takes to notice a difference in the weight gain and brain fog? I’m assuming since it was a gradual process for my body to start storing fats that it’s a gradual process to stop storing them as well. Thanks for your help!
Thank you for this.. My Dr. just recently suggested gallbladder removal because of my intense heart burn… I will definitely NOT go along with his suggestion.. Too many doctors are jumping the gun nowadays and performing unnecessary surgeries and then having the patient suffer the consequences down the road.
Thxs for this info.
I’m already overweight. So worry bout my health too.
Pls guide me which supplements I can take.
Can I take Herbalife for controlling weight.
Thxs once again
I had my gallbladder removed in 2014 because I had a gallstone shoot out into my pancreas. Caused severe pain under my left breast. I thought I was having a heart attack. At first they told me I had gallstones but they weren’t going to bother them because they didn’t see a problem with them. But they didn’t know what cause my pain, then they decided it was a gallstone that shot out. That is when they decided to take out my gall bladder. They did an MRI to make sure the stone wasn’t still in my pancreas, and didn’t see one. So during surgery they inserted another opening in the center just below my breast to look around to see if there was a loose stone. They continued to remove my bladder after they saw no loose stone. They gave no information on what to do afterwards. I started gaining weight imediatly after that all in the stomach. I have been on a high protein, low carb diet since Febuary 2016. I have lost about 15 pounds, but I still have my big stomach. I have been taking Beta plus now going on 3 months, but really can’t tell much difference. I have a feeling my big stomach is here to stay. Good luck on your problems.
Wow! How I wish I would have had this article years ago!
I had my gallbladder removed at the age of 16 (the second youngest patient in the hospital to do so) and I was NEVER told about any symptoms after it’s removal. In fact, I was told that “the gallbladder does little to nothing really…” Had I known then what I know now, boy would it have been different.
After my surgery, I was told that it would be a little while before I “bounced back to normal.” Now, I’m not saying that I was really skinny when I had it removed, but I was no where near being over-weight. By the time I was 19, I became the heaviest I have ever been. It was the biggest struggle of a life time.
Once I went off to college, I was able to lose some of the weight by constantly walking everywhere, moving heavy equipment (art major), and eating less fatty foods I was able to work off a lot of excess weight and become just ‘over-weight’ again.
At this point I have been able to keep my weight the same, not losing anything, but definitely not gaining any either. I have been getting so annoyed that I have tried EVERYTHING from extreme dieting and exercising to no avail. So, thinking back to what led to this and really wanting to know if lack of a gallbladder was doing anything to me, I found this article.
Totally makes sense!!! I want to thank you for this. I know that I will begin another attempt at getting healthy, this time on the right foot.
I have gallstones I am suppose to get my gallbladder out but have not yet,I had one attack an I think it was do to pregnancy? It happen a few months after giving birth.I also have pcos but have it under control but gained so much being pregaunt I need to lose weight,afraid to take out gallbladder an afraid off an attack to keep it in,will ur pills set my gallbladder off? Please help,doctors say take it out,I have 3.
Hello,
I’m so desperate for help i’m going crazy. I’m only 19 and I can’t stop gaining weight. I get extreme pain whenever I eat and nothing will stop making me look like a huge whale. I started the school year at close to 157 and I have been good all year. I eat gluten free, I never eat junk food (literally never) I eat salad, I eat rice, I eat fish, i’m almost the definition of a perfect eater yet now I’m only a couple pounds away from 170. No matter working out or not I gain weight, I need help! I want to lose weight so desperately and can’t. I think it has something to do with my gallbladder but after reading all these comments I don’t want it taken out just to gain more weight! Please anything will help.
Thank you.
Hi Abby… Have you had your thyroid checked? This sound like what happened to me about 13 years ago. I literally started gaining weight over night.. With every pound I was working out more and eating better but the pounds kept coming on.. Within a couple months I had gained 40 pounds.. That is when I was diagnosed with hypothyroid.
I agree with your article. I too believe each part of our body was created for a reason including the gallbladder. I had put weight on for 2 years and after the birth of my first baby I had my first confirmed gallbladder attack where I was rushed to hospital. Although I suspect there were many other signs ignored as pregnancy symptoms. I was scared of surgery, and the surgeons were very patient giving me the option to change my mind for the next year. But with statistics that suggested I would still have the same symptoms after, I read between the lines that I would have more weight gain problems and I was just plain scared. So I told myself this wouldn’t happen again and refused surgery. But it did. Over the coming 6 years it steadily increased each time I was rushed to hospital. I made deal after deal with myself, I could cope with once every six months, then once every 3 months, then once every 2 months. I gave up meat and then I told myself I could live only on tomato soup and apples so as not to upset my gall bladder. Until finally a stone blocked the duct. I even ignored it then, I was in constant pain for 5 days unable to eat anything. I was terrified. The doctor saw my eyes were yellow and my urine was very dark. They sent me to the hospital where I was told I was in early stages of liver failure. All I wanted was to go home and look after my new baby and my other kids but I had to face this. That’s the point I had the surgery. Yes I have put on weight but no I don’t have any symptoms like I did. I no longer go to the hospital and I feel normal again just fatter. I need to fix that and I don’t know how but if I had the decision again I would have had the surgery at the start.
I am,43 I have never weighed over 130lbs all my life I am a SICKLE CELL patient I was just told today I have no spleen and I have lots,of gallstones I will have surgery April 21st 2016 I weigh 108lbs I hate my ,weight loss I understand lots of,people struggle to lose and I’m dying to gain.
hi . i have gullstone . i am 18 lost 30kilos bt still am 74kgs for the past 2 years n cant seem to lose the last 15 kilos no matter wht . wht kinda diet will help me lose the last 15 kilos
i have many symptoms.
don’t want surgery at all.
what else can be done.
side effects from surgery sound horrible.
Thank you for this article! I had my gallbladder removed in October 2014 and had significant complications related to a bile leak following surgery. My diet is clean, and I exercise regularly. I was 140 then and am 190 now. I have tried just about everything to take this weight off, and I’ve been extremely unsuccessful. Other than the supplements recommended above, do you have any other suggestions?
Nice Article. Sadly you are 100% correct, every gallbladder surgery is carried out in a manger that is medical fraud, informed consent is never given as risks are never presented. Leaving a post operation patent with no information on how to survive without a gallbladder function is intent to commit harm. The stories (mainly from woman) finding their health failing before their eyes is sickening to read. Thank you for speaking up against main stream medical opinion , that the gallbladder is non essential organ, not required to live a healthy life, which we know is a lie as there is NOT a single medical studies known to mankind that can back this quackery . More sadly, the doctors who had all the answers ‘ remove the gallbladder’ have no answers when the problems start to kick in. New Zealand surgeons have gone on record and advised weigh gain is not a post complication of removing gallbladders and their function. They have also stated post cholecystectomy syndrome is simply controversial, so no health risks are presented when obtaining consent for the procedure. This is backed by The New Zealand Health and Disability Commissioner, who ruled Surgeons are not committing medical fraud by not disclosing likely post complications. And holds a contrary to many medical studies and non surgeons opinions, he states there are no likely heath complications from removing gallbladders. Backed by the Health Commissioners rulings, ever gallbladder surgery procedure carried out in New Zealand is carried without providing informed consent. A direct human rights violation . Also, As no problems exist, public hospitals will not provide post care problem support either. Surgeons have even presented the Health and Disability Commissioner ruling to prevent post care support. Sadly little hope for many patents in New Zealand post removal
What a good read. I had my gallbladder out due to a blockage, acid went back into my gallbladder and made it spongy. No one mentioned weight gain and that I would have times when it feels like food is just sat in my stomach going no where and other times when 5 mins after I’m on the loo. Drs don’t tell you how you are gonna be after the op, just that you won’t have any pain, and that’s a lie. Wish I had read this earlier and maybe I could have looked at the removal differently. My op was in2012 and my digestive issues are still on going.
Hi I don’t have any fb account so can you please tell me here which products do i have to take to get rid of this weight gain..i have been taking hell lot of weight loss medicines since years but nothing seem to be effecting me..i am 26 and almost 12 kgs overweight..please help me miranda..
You don’t have to have a facebook account to order. Simply click on the SHOP tab on the front page of http://www.mirandajorgenson.com and you can purchase any of the products I most frequently recommend. Should you choose to make yourself a facebook account though, we have a wonderful community there that shares a lot of health information. It is called Weight Loss Resources with Dr. Miranda
I had my gallbladder taken out in march 2013 and weighed 138 pounds for 10 years by may 2013 I gained 20 pounds and keep gaining weight April 2015 I weighed 160 now im up to 180 and been to 9 doctors who all tell me this is normal
I changed my diet didn’t help I even took adipex didn’t help I’m at loss I can’t gain anymore weight
I had insane pain under my right lower rib. I had a ultrasound of my gallbladder and was told it was packed with stones. I was told it could burst. I was not advised of any problems that could happen. I was told a fairy tale. “I would be pain free & be normal. The surgery was same day. It was 15 day Hospial stay. Five days in icy and bleeding due to a cut in my liver. I have gone from 140 to 190 and feel like hell. I still have pain, not as severe, yet my quality of life has taken its toll on me both medically and mentally. I’m angry at my Surgeon. I feel screwed over.
I’m a proud Marine who stayed fit. I am feed up. Even after getting discharged, I beg you for help.
Semper Fi
Alan Alswang
PS; keep me up to date on what steps I could take to lose weight and return to a semi normal life.
If I take bile acid/salts for better fat digestion, will my Cholesterol and Triglyciride numbers get worse?
I have to Thank you for providing this eye-openIng info! Just have that lingering question. My gallbladder was removed in 2008 and I was under the impression that any excess fat that I couldn’t digest and use would just bypass digestion and take the Fast track to the exit. Since surgery my cholesterol and triglycerides #s are terrible, don’t understand since the fats aren’t digested. Your explanation of Starvation mode makes sense, but I’m concerned that my numbers might get even worse once I start taking bile acids and actually digest the Fats. I hope you have the time to answer and Thank you for your time.
Your lipid panel should improve rather than get worse
I have had my gallbladder taken out, recently I had a baby and trying to lose that post baby weight has been a nightmare. I have worked hard at it, I have always been athletic, but to lose the weight I worked out four times a day, I also kept a strict healthy diet, two months later I saw no progress, not even a little, so I turned to the garcinia Cambodia, pills and also fit tea, hoping the ads were true, I took them both faithfully with my diet and exercise, but nothing. I wonder if having my gallbladder removed is why it just won’t budge? Thanks for the article, it was a good insight on what might be going on.
Miranda I found this page because I was actually searching for solutions on healing the gallbladder sludge. But unlike most of the people on this post I’m the opposite. Im 92lbs and I cant seem to gain weight. It seems like almost everything I eat is creating gas and pain and I get nauseated if I eat alot of oil or fried good. I get pain in my shoulder blades and in between them as well and the pain is always on the center to right side of my stomach. My nutritionist told me that she thinks I have sludge in my gallbladder. I dont know what to eat or what to do to feel better and gain weight. Ive never been this unweight before even when I was a vegan! I’m taking zypan and that helps but should I do everything you suggested even tho im underweight?
My dearest friend found your site, due to the concerns she had for my health.
My gallbladder was removed in Sept 15, before the op and continuing after and even now, I have gained weight, am in pain especially after eating, and yes, it is just right of middle under my lower rib.
I have exercised and been on a low fat diet, but my weight fluctuates from losing 2 lbs to putting on 5.
I am snappy, depressed, indecisive, all the symptoms you describe I have, so I thank you for the explanation, and I amgoing to change my diet and supplement.
I am waiting for my surgery date to remove my gallbladder. I have been diagnosed with mobile multiple gallstones, I had gained weight over the last year, a lot, eating more paleo and healthy fat foods! now I can no longer eat them, my weight wont stay on. Scans and cameras have ruled everything else out, all bloods are perfect as under haematology for a rare disorder, so its the gallbladder.Sadly I am one of the few I think needs it. Several women have needed it removed in our family, despite all having different lifestyles and dietary needs/plans. I have worked alongside 2 naturopaths now for several months but getting worse. It is causing reflux, IBS symptoms, nausea, bruised ache in right lower rib, gas, pain after eating and feeling bloated. I was paleo 90% for many years prior and my diet was full of healthy fats, coconut, organic meats, nuts and seeds and LOTS of raw veggies, sauerkraut and now I have had to remove most foods to keep symptoms minimal and lost 15kg, almost underweight now and eating very dark chocolate despite the slight burn and organic gmo free corn chips to stop the weight dropping! I never ate fried or takeaway, ate lots of fermented veg, dandelion root tea, kefir and turmeric, so should never of got them in the first place. I hardly ate gluten, only once a month on date night as nan bread at the indian or bun at the healthy burger joint or occasional pizza, depending where we decided to date night and otherwise a little cheese and cream with cooking and sourdough organic kamut bread ( whole loaf lasted a month, so hardly any)I have now been gluten and dairy free since October, heaps of liver and gallbladder supplements, tried chanca piedra tea, use digestive enzymes, probiotics, ox bile supplements. I have tried slippery elm, been on magnesium supplements and still getting worse, still cannot ohld weight and my once 3/4 healthy plate and diet is now a lot worse and poor in comparison but eating what I can to keep weight from continuously dropping and producing minimum symptoms. So I have given up and I am booked for surgery ? I live on chicken and rice, very little cooked veg ( most veg raw causes me pain and digestive distress) berries, coconut yogurt ( seem ok with this) hardly any nuts as they give me IBS symptoms and a few seeds.
Totally trying this. Had it out years ago and I am religious about exercising and nothing works to shake off that last 20 pounds or so. Also constantly getting sick all the time and I know I am not absorbing anything and losing my hair like crazy to boot. Doctors don’t seem to care honestly and its really frustrating. Just taking probiotics and vitamin is all they suggest and its not working.
I had my gallbladder removed 3 years ago. Since then I pass large amounts of mucus, my stool is yellow, bloating, 25 lbs weight gain, and a lot of diarrhea. I saw GI. Colonoscopy completed and only a dx of IBD. Yet symptoms still persist. The weight gain has severly affected my life. Any thoughts?
Feel free to message me privately and I’d be happy to discuss this with you