by drmiranda | Sep 22, 2015 | gallbladder, health, weight gain, weight loss
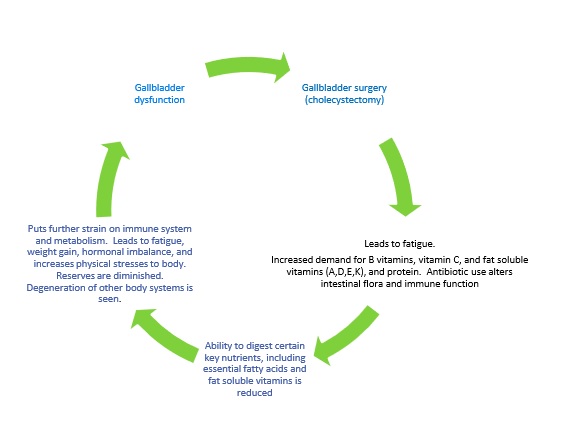
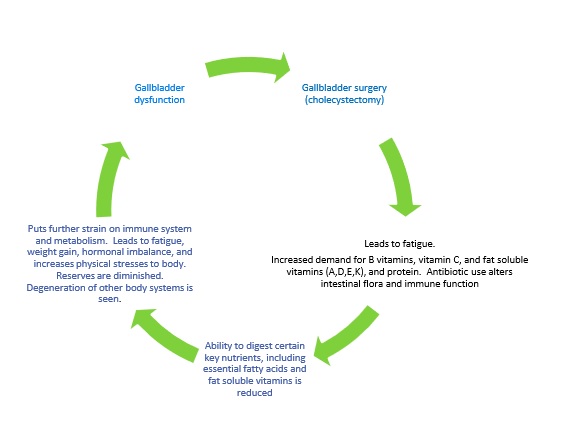
This basic principle applies to any surgery , albeit different organ systems are affected, but for our purposes, we will relate this to gallbladder surgery (cholecystectomy).
ANY time you have surgery (of any sort) you can experience fatigue. Your body only heals when you are asleep – so that is nature’s way of getting you to slow down – so you can heal efficiently [while sleeping]. That said, most people didn’t go into surgery with a fully functioning gallbladder. It could have been dysfunctional or essentially non-functioning for months or even years before that. So , that means you have months or years of digestive issues and not getting the building blocks your body needs to make hormones or repair itself. Surgery brings its own issues, as it increases the demand you have for certain nutrients – like vitamin C, B vitamins, protein, glutathione, etc . So, when you have gallbladder surgery – you go from just being deficient in the fat soluble vitamins (A,D,E,K) and essential fatty acids to being potentially deficient in most of the major vitamin categories. To compound matters, they typically put you on a significant dose of antibiotics after your surgery – which kills off the good bacteria in your gut along with the bad, and since 80% of you immune function comes from the gut and those good bacteria, your immune function goes down , making your MORE tired and susceptible to catching everything that goes around. It is a hard thing to dig yourself out of. You have to overhaul your diet (and you rarely get that advice), you have to get optimal levels of sleep, and you have to get out in the sunshine and fresh air and get some exercise. Otherwise you feel like you are trying to dig yourself out of a hole with a plastic spoon. Now, occasionally people feel great after surgery, but they are the exception to the rule. In 12 years of practice, I have rarely met anyone who didn’t have to make changes to feel better afterwards. Sooner or later their underlying nutritional deficiencies caught up to them and affected their health.
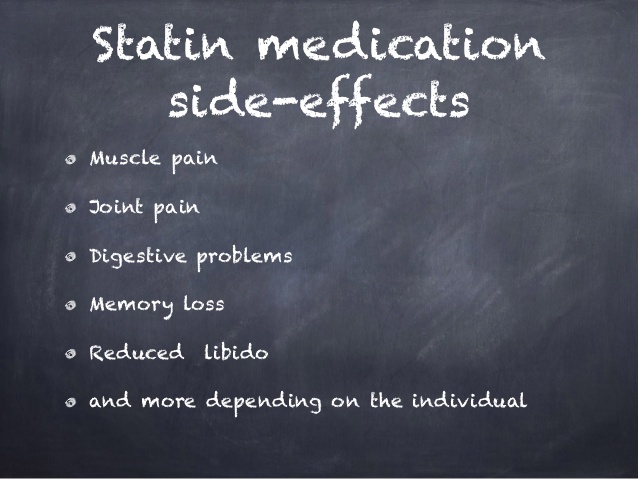
Your body uses cholesterol and vitamin D as precursors to make many of your hormones, including your sex hormones. Fats are necessary for life, and your brain is largely a fatty organ. This is why people taking anti-cholesterol medications (statins) frequently experience decreased libido, or even sexual dysfunction. They also often experience short term memory issues. 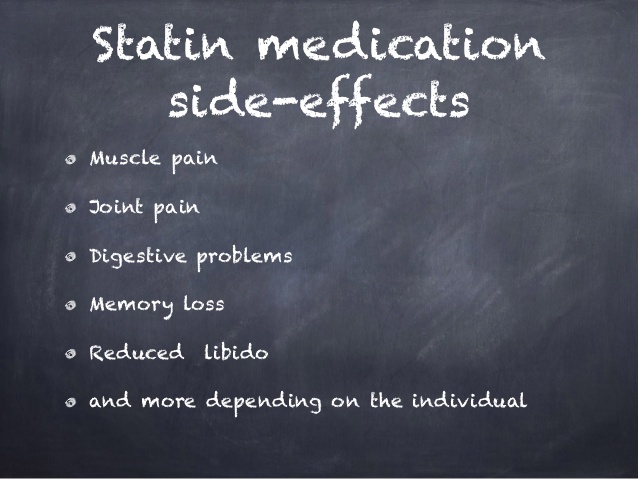
I have heard doctors argue that the gallbladder is unnecessary. They say that since the liver continues to make bile, then fat absorption continues. I disagree with this. First, I don’t believe we were designed with unnecessary parts. We may not realize their full worth or function yet, but that is a human limitation, not a limitation of our creation. Science only ‘discovered’ what the appendix was for within the past few years (It acts as a reservoir for healthy bacteria to recolonize our intestines after fever or illness). Since cholecystectomy is one of the most commonly performed surgical procedures in this country, it makes sense that there is more money in removing them than figuring out how to save them. But I digress, let’s get back to the liver making bile – it does keep making it. The level it makes it is dependent on whether you have fatty liver degeneration or not. But let’s say that you don’t have fatty liver — the liver is going to drip, drip, drip 27-34 oz bile out in a steady stream. That bile is very caustic, and would normally be funneled over to the gallbladder where it is collected and concentrated, up to 18 times – down to 1-3 oz. It is this highly concentrated bile that is designed to break down the fatty acids and fat soluble vitamins you consume. The pre-concentrated bile, while caustic and irritating to your gastric mucosa, can’t hold a candle to the concentrated bile your gallbladder should hold. There is never enough, and never enough at the specific concentration required to absorb those key nutrients out of your diet. So you become deficient and your body goes into conservation mode. Some experience this immediately, others find it takes 6-24 months to fully start experiencing the effects. People find it harder and harder to lose weight, or they find themselves gaining weight despite eating the same diet they always did, or exercising. They find they get fatigued easier, and that they are more susceptible to colds and flu. If they have autoimmune disorders, they may find themselves experiencing a greater degree of symptoms.
So what can you do? I will be the first to admit that I don’t have all of the answers. If anyone suggest that they do – RUN! I can tell you that what my research, and my experience has led me to works for most people. First, you need to keep a food journal and track every meal you eat and how you feel afterwards. Gas, bloating, and diarrhea are the most commonly experienced repercussions from having cholecystectomy. 1 in 15 people who have had their gallbladder removed experience Habba Syndrome, which is commonly misdiagnosed as IBS, or even Celiac Disease. 5-40% of cholecystectomy patients will experience post-cholecystectomy syndrome (persistent right upper quadrant abdominal pain, bloating, gas, nausea, diarrhea, and general malaise). Often, these people will know the whereabouts of every bathroom in their vicinity, because they experience issues almost immediately after eating. Dietary changes will be necessary. Certain foods aggravate a significant number of people with no gallbladder. These include greasy foods, carbonated beverages, dairy, and simple carbohydrates. Wheat products, including breads and beer, can also elicit a negative response. Please don’t take this as a reason to stop eating healthy fats — you NEED to consume them in order to maintain your health and shift your waistline. Use specific dietary supplementation to replace some of the action of the gallbladder. I recommend a blend of ox bile, beet concentrate and pancrelipase to substitute for this action. If you avoid fats, you will make matters worse. Since digestive enzyme production decreases with age, if you are over 40, adding digestive enzymes to your meals can also cause significant relief. make sure you are getting adequate levels of sleep so that your body can repair itself and so that levels of stress hormones can decrease.
- Keep a food journal to log your physical responses to foods and beverages. Learn what your body can and cannot handle.
- Use specific dietary supplements to increase your digestion and resolve your underlying nutritional deficiencies.
- Get 7+ hours of uninterrupted sleep per night.
- Get out there and move. Aerobic activity and weight bearing exercise is crucial for your recovery. Walking is a great way to get started. Walking in the sunshine is even better (get some vitamin D while you are at it!)
Image courtesy of Ohmega1982 at FreeDigitalPhotos.net

by drmiranda | Sep 1, 2015 | blood test, fatigue, health, hypothyroid, inflammation, insulin resistance, not losing weight, obesity, weight loss
You’ve heard about preemptive strikes, how about preemptive health? Don’t wait until you are really sick to get blood work drawn. Have it drawn at your yearly physical and keep a copy for your records. You OWN your medical records, by the way, your physician is just the custodian of them – so you are legally entitled to a copy of anything contained within it.
PREEMPTIVE HEALTH: What Blood Work to Request from Your Doctor
I get a lot of requests from people asking what blood tests they should request at their next medical appointment. Along with getting a standard Chemistry Panel and Complete Blood Count (CBC) which should include RBC Magnesium and RBC Potassium , here are the ones I commonly recommend for women. Men would have a few slight differences.
1) Complete Thyroid Panel :
TSH (many doctors only test TSH, and that is like trying to diagnose what is wrong with your foot by only looking at your big toe)
Free T3 (also known as: Triiodothyronine, Free)
Free T4, Direct S (Not Free T4 Index, Free T4 calculated, or TSH reflux)
Reverse T3 (If your doctor will do this and/or if it’s available in your country)
***Because this test includes a TSH screening, remember that medications like corticosteroids, aspirin and lithium can interfere with those results. Also, if you’ve had a recent X-ray that used iodine dye – or other radioactive tests – ask your doctor when you can take an accurate TSH test. Pregnant women in their first trimester should also ask their doctor about the proper time to get a TSH test.
If you have symptoms of hypothyroidism and/or Hashimoto’s Disease, add these :
Thyroid Peroxidase Antibody (TPOab)
Anti-Thyroglobulin (TgAb)
If you have symptoms of hyperthyroidism (much less common), add these:
Thyroid Stimulating Immunoglobulin (TSI)
Thyroid Receptor Antibody (TrAb)
2) Iron panel:
Serum iron
Total Iron Binding Capacity (TIBC)
%Saturation
Ferritin
3) Vitamins:
B12
D3
4) Sex Hormones (serum blood):
Testosterone
Estradiol
Progesterone
FSH
LH
DHEA
***The sex hormone tests should be done 7 days after ovulation. If you don’t know when you ovulate, an ovulation kit can be purchased from a drugstore, or you can just test on day 21, if you still menstruate. If you no longer cycle, the tests can be done anytime.
5) Other tests:
C-Reactive Protein (systemic inflammation marker)
Cholesterol panel ( I don’t care if it is high, I look at the ratios, and your CRP level^^^)
Fibrinogen (clotting & inflammation marker)
Hemoglobin A1C (long term measure of glucose status)
Homocysteine ( risk for coronary artery disease, fractures, and other disorders)
################################################################################################
A) If you have ANY chronic health conditions, I recommend getting an ELISA Food Sensitivity and Allergy Panel done. It is an easy way to identify what you consume that is contributing to your systemic inflammation. Most family doctors do not perform these tests, you will need to go to someone familiar with them. ALCAT and ALLETESS are the two brands of testing that I have used with my patients. Their respective websites can help you locate a practitioner who is versed in them www.alcat.com , www.foodallergy.com
B ) If you have symptoms of low cortisol/ or adrenal fatigue, then salivary cortisol tests should be considered. Cortisol levels: 24-hour saliva cortisol tests from Canary Club and MyMedLab are done through ZRT Laboratories: http://www.canaryclub.org/diurnal-cortisol-4x-stress-hormone-kit.html ($119+shipping) or https://sttm.mymedlab.com/sttm-profiles/sttm-24-hour-cortisol-dhea ($125)
Symptoms of low cortisol: http://www.stopthethyroidmadness.com/adrenal-info/symptoms-low-cortisol/
C) Educate yourself! Read up on what you are experiencing: Books I highly recommend: Type II Hypothyroidism, Dr. Mark Starr; Stop the Thyroid Madness, Janie Bowthorpe; What is Your Menopause Type? Joseph Collins ; Death to Diabetes, DeWayne McCulley, The Blood Sugar Solution, Dr. Mark Hyman; The Adrenal Reset Diet, Dr. Alan Christianson; Hashimoto’s Thyroiditis, Wentz & Nowasadzka.
©2015, MirandaJorgenson, www.mirandajorgenson.com
by drmiranda | Jul 15, 2015 | blood supply, diet, dietary supplements, fat breakdown, fatigue, health, insulin resistance, lipolysis, not losing weight, plateau, walking, water retention, weight gain, weight loss
This is an aspect of weight loss that perplexes a lot of people – they start a new diet and notice their clothes getting looser, or their face getting thinner – but their weight is staying the exact same! It is frustrating, because you *think* your diet is working but you step on the scale and feel like a big old failure.
Well, I am here to tell you that you can relax! You are not a failure! You are experiencing the wonders of the fat cell in action (I can hear you saying, “big whoop — skinny thighs are what excites me!”).
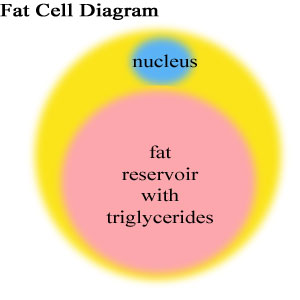
Let’s start off with a little physiology lesson. In your body you have 10-30 billion fat cells, and that is if you are of a healthy weight. Overweight people can have 75 billion fat cells or more, and it is not unheard of for morbidly obese people to have 250-300 billion fat cells overwhelming their boney frames! That is a LOT of fat cells (adipocytes). Picture each fat cell like a little deflated balloon. That balloon can be relatively empty or filled to the brim and be stretched over 10x its normal size. Now these fat cells are stubborn creatures – you can always make more, but once you have them, they are yours for good. Up until very recently1, it was thought that the only way to get rid of fat cells was to cut them out, but you can deflate them — and this is the key to losing weight effectively.
You see, fat cells are little storage tanks, and despite your most heartfelt desires to the contrary, they are remarkably efficient at storing fat in the form of triglycerides within the cell. When we want to burn fat – it isn’t an easy matter of having your brain tell your body, “we need more energy – let’s burn that love handle”. It doesn’t work that way! We need two enzymes, hormone sensitive lipase and adipose glyceride lipase to break down the triglyceride within fat cell where it is then released into the bloodstream as FFA’s. The more blood supply an area has, the better it can whisk away those FFA’s that are getting dumped from the fat cells. You can see this on your own body — take a second and poke your facial cheeks. See, the fat there is nice and soft because it has a good blood supply. Now grab the fat on your belly or on your butt. Feel the difference? It is dense and hard. It doesn’t have a good blood supply to whisk fat away. This is why when you start losing weight, it usually leave the ‘soft’ places first – your face, breasts, and arms and leaves you feeling like a saggy humpty dumpty for a while. This blood flow issue also leads us to our key point – when you start a diet and are burning fat, the scale often stays immobile despite you noticing that you are shrinking. This happens because the body abhors a vacuum. When the adipocytes dump out their fatty contents, your body doesn’t like to see an empty cell – so it shuttles water into the cell to fill up the space the fat just occupied. This is also why fat loss can be considered an inflammatory process and why you often feel bad, tired, sick, or swollen when you are dieting (there are other chemical factors, but we will discuss those at another time). Your body is literally replacing the fat with water! This process is more extreme for some people than for others, and some fortunate souls experience very little of this water replacement. This is also why your stomach or thighs can feel mushy or spongy when you are losing weight – you are replacing a dense fat with water.
So, what you can do, especially if you know that you have resilient fat or are a water hoarder? Well, there are a few simple things:
- Stay hydrated. I know, you’re thinking, “Why put more water into a swollen body?”, — Well, you need to flush out the metabolites from breaking down those FFA’s.
- Limit Caffeine and Alcohol. A little of either substance is OK, and small doses of caffeine can even be beneficial because it has a mild diuretic effect. Large amounts of either (and by large I am referring to more than 3 caffeinated beverages or more than 1 glass of wine or beer each day) can cause you to swell up like a balloon at the Macy’s Day Parade AND make your hard-earned weight loss come to a grinding halt.
- Shake your booty. Yes, I said it. The largest lymphatic pump in your body is the quadriceps muscles in your legs, so anything that gets those quads pumping — like walking, dancing, or biking, increases your lymph flow and your blood flow. If you work yourself up to a decent exertion point, then you will really increase systemic blood flow, and breathing (and breathing is the means by which your body excretes the metabolites of burnt fat cells!). Dig out those Richard Simmons’ shorts you’ve been hanging onto for the past 20 years — (they are back in style) and get ‘Sweatin’ to the Oldies!’
So there you have it! Know that you are not hallucinating – your face is thinner, your breasts are shrinking, and those bingo wings are real. Your scale just hasn’t caught up with your body! The more you follow the above steps – the faster you will purge that excess water (and inflammation) and the scale will start moving in the right direction.
1.http://www.nytimes.com/2008/05/05/health/research/05fat.html?_r=0
by drmiranda | Jul 7, 2015 | health
We focus a lot on people that have had gallbladder removal surgery (cholecystectomy), but most people who have underwent gallbladder surgery, didn’t get to that point overnight. They likely experienced symptoms associated with gallbladder dysfunction for months or even years prior to undergoing the knife!
Symptoms of an improperly working gallbladder:
It is unlikely that you will have all of the following symptoms, but it is probable that you will have more than one of these symptoms if your gallbladder isn’t working at 100%. You may not have symptoms constantly or even consistently however. Up to 70% of people with gallstones do not have extreme symptoms and the gallstones are found during check-ups for other conditions. many people think that gas, bloating, indigestion, or constipation is *normal* for them, and they do not associate it with an improperly functioning gallbladder.
| Gas |
Bloating |
| Indigestion |
Bile reflux |
| Constipation |
Diarrhea |
| Nausea after eating |
Fatigue after eating |
| Headaches after eating |
Shoulder pain (left) |
| Colic type pain |
Belching |
| Light colored or floating stools |
Frequent hunger or cravings |
| Weight gain, or inability to lose weight |
|
Who is at risk for developing gallbladder dysfunction?
With our Standard American Diet (SAD) it sometimes appears that everyone is at risk, but certain populations are more at risk than others. Here is a list of things associated with gallbladder dysfunction and disease:
| Women, increases for those who have kids |
40+ years of age |
| Obesity |
History of bariatric surgery |
| Hypothyroidism |
Food sensitivities and/or allergies |
| Elevated cholesterol |
Ethnicity (Native Indian, Mexican, and Asian) |
| Habitual Dieters |
Alcohol intake |
| Diabetes, insulin resistance |
Inflammatory Bowel Disease |
| PCOS |
Menopause (especially with HRT) |
| Lack of exercise |
Pregnancy (due to increased hormones) |
| Use of antacids, PPI’s |
Extreme diets of any type |
| Family history of gallbladder disease |
Low stomach acid (hypochlorhydria) |
| Use of antidepressants |
Use of cholesterol medications |
| Use of immunosuppressive medications |
People with chronic heartburn |
| Gluten intolerance |
Use of HRT, estrogen, or progesterone |
| Smoking |
|
What can you do to take care of your gallbladder?
You could write a book on all of the things that one could do to help their gallbladder function optimally, so for the sake of brevity, I will keep this list short and expand on it at a future date.
- Avoid extreme diets and QUICK weight loss. Slow losses are much safer
- Moderate alcohol intake is protective against gallstone formation, however drinking more than 5 drinks a week increases your risk. Moderation is key.
- Regular vigorous physical activity, such as walking after meals is protective.
- If you are diabetic, keep your blood sugar under control
- Eat a healthy diet, avoiding processed foods
- Make sure to consume adequate amounts of protein
- Consider supplementing with bile acids, beet extracts, pancrelipase, digestive enzymes, vitamin C, magnesium, lecithin, peppermint oil, artichoke, etc.
- Consider taking digestive bitters, or chewing a piece of a bitter herb (even parsley) prior to eating. The bitterness triggers your gb to work more efficiently
- Drink tea
- Eat more vegetables, particularly those known for their fiber content
- Make sure healthy fats are a part of your daily diet
- Consider IgG and IgE blood allergy testing for food sensitivities and eliminate trigger foods
- If you take medications known to exacerbate gb issues, speak to your physician about alternatives
When all else fails…
Cholecystectomy is one of the most commonly performed surgeries in the united States and is one that could largely be avoided in many people. There are cases in which the gallbladder clearly needs to go due to infection, cancer, or other issues — however this is a decision you should make after receiving a fully informed consent from your physician. If you have any doubts, or you feel pressured – please seek a second opinion! I would like to note that the British Medical Association cautions its physicians to educate their patients that cholecystectomy is associated with weight gain in 68% of women and 87% of men! 1 In another long term study of women post-cholecystectomy, only 11.1% were able to maintain their weight within 5 lbs over a 16 year follow-up period.2 Despite this obvious association, few American physicians appear to educate their patients on this very real side effect of gallbladder removal. In fact, many patients are told that there may be some ‘digestive discomfort’ for the first 6 weeks post-operatively, but after that they will have NO SYMPTOMS. This however is not my clinical observation, nor the reality of most of the people I have consulted with. Lastly, I would urge extreme caution to anyone considering ‘gallbladder cleanses’ that are promoted heavily on some websites. Not only have these flushes whereby people consume a low-fat diet for several days then drink a lemon juice/olive oil mixture under the guise of eliminating gallstones, been proven to be ineffective (studies show that the hardened blobs eliminated are saponified fats, not gallstones) but they can be very dangerous and causing extreme stress to a gallbladder could dislodge an asymptomatic stone into a bile duct and result in the need for emergency surgery!
Please see my post Is your gallbladder (or lack of) stopping your weight loss? for further information about post-cholecystectomy issues and weight gain.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1443570/?page=1
- http://www.ncbi.nlm.nih.gov/pubmed/10075614
by drmiranda | Nov 26, 2013 | diet, dietary supplements, fat, health, obesity, plexus slim, Plexus Slim Doctor, Uncategorized, weight gain, weight loss
There is so much information and misinformation about weight loss on the internet that it is hard to wade through it all. Everyone has a different theory – it is fats, it is carbs, it is meat, it is dairy, it is preservatives, it is too many calories, it is not enough exercise, it is an inevitable part of aging, it is estrogens, it is not enough testosterone, it is mercury in retrograde… blah, blah, blah… Surely someone must have some answers!
Well, ten years of nutritional practice has taught me that no one has all of the answers. If you find someone who claims otherwise – RUN the other way! Weight loss science is constantly changing and it is as mercurial as the people who espouse individual diet plans. Quite simply, there is no quick fix and there is no single plan that will work for 100% of everyone. Period.
What I can tell you is that there are certain hormones that play key roles in many people’s weight gain or inability to lose weight.
1. Your body is not producing enough adiponectin. Adiponectin is a protein specific to fat cells and it is believed to play a role in the development of insulin resistance and atherosclerosis. Typically, the more body fat you carry, the lower your adiponectin levels, with increased levels of visceral fat (that fat hidden in your abdomen, packed around your internal organs) being especially correlated to decreased levels of adiponectin. Almost every symptom associated with metabolic syndrome or insulin resistance can be directly tied to adiponectin, so – how do you make more of this hormone and head off these problems? First, you need to increase your magnesium intake with supplements (like BioCleanse, or magnesium glycinate) and magnesium rich foods (raw spinach, pumpkin seeds, nuts, seeds, beans, lentils, fish, brown rice, bananas, figs, avocados, dark chocolate, etc.). Second, you should look into fish oil (omega 3 fatty acid) supplementation and exercise to increase your adiponectin levels.
2. Insulin imbalance. Think of insulin as a key that unlocks your cells so your body can take the glucose (sugars) in your blood stream and store it away in the cell for later. If you don’t have enough insulin, your circulating blood sugars remain too high, and these negatively affect your vasculature system, your fat storage, your blood pressure, your ability to heal, and even your brain. Much of the medical community thinks that insulin resistance stems from the body not having enough insulin, but other researchers, like Dr. Mark Hyman, MD, believe that too much insulin is the problem. He postulates that elevated levels of circulating insulin are even more problematic, and that many of the drugs and methods used to treat elevated blood sugar levels , actually cause the body’s tissues to be flooded with too much insulin, which slowly cause your body’s cells to become resistant to it, which means that greater and greater levels of insulin are needed to see any effect, which leads to vicious blood sugar and insulin swings, making these hormones rollercoaster throughout the day. The ingredients in Plexus Slim support the normalization of your insulin resistance. In addition, some studies have shown that consuming 2 tbsp. of apple cider vinegar before a high fat meal may work as well as drugs at decreasing blood sugar levels. If you consume artificial sweeteners, do yourself a giant favor and STOP!
3. Too much ghrelin. Ghrelin is your hunger hormone and it is found in the cells that line your stomach. It stimulates the hunger center of the brain and makes you desire sweet or rich foods. In fact, it is so efficient at stimulating your hunger centers, that elevated levels of ghrelin will make you feel the same way as if your were in full starvation mode – desperately craving the richest, highest calorie foods you can imagine. Furthermore, it makes you feel unsatisfied with the amount and quality of food you have eaten, whether you are truly full or not. It’s why you can slip in that piece of pecan pie or chocolate cake for dessert when you are already uncomfortably full from eating that big turkey dinner. A classic sign that you have too much ghrelin is that you feel you have room for dessert, or you find you are a bit hungry an hour or so after you eat. You fridge-cruisers know who you are! Ghrelin cycles in 4 hour increments, so typically you would be hungriest 4 hours after your last meal. So how do you address ghrelin? There are a few different things you can do. First, make sure you are getting enough sleep. 8 hours of sleep per night is the ideal. If you are getting less, or have poor quality sleep, please know that sleep deprivation causes your ghrelin levels to increase. Protein intake also staves off the release of elevated ghrelin levels, so make sure that each meal starts off with high quality protein sources (this is particularly important for breakfast). Consuming a small bowl of broth or soup before a meal is an excellent way to prevent ghrelin levels from rising too much.
4. Cortisol overload. We are designed for fight or flight. Cortisol is produced as a response to stress (and who isn’t stressed nowadays?). It increases your cravings for sweets and carbohydrates, it increases muscle breakdown for energy production, it increases the percentage of fat that is stored in your abdominal area, and it increases your levels of depression and anxiety – which make you eat more, which further increases your cortisol levels, creating a vicious cycle, resulting in you feeling tired and burnt out all of the time. Supplements such as fish oil, Rhodiola, lactium, magnesium, DHEA, and b-vitamins can all help reduce cortisol levels. Other things that have a positive effect include slow exercise like yoga or walking, meditating, praying, or just getting into a ‘zone’ where you let your creativity reign. Limiting coffee, and making sure you get enough sleep are other ways to keep cortisol levels normal.
So before you give up he fight, have a good look at these factors and see which ones may pertain to you and take the action steps needed to achieve your ideal weight. I have found Plexus Slim to be an excellent tool for my patients and clients in achieving their ideal weight in a safe and efficient manner. It truly is the non-diet, because it never involves meal replacements, shakes, calorie counting, points, or anything else. It simply helps to normalize insulin resistance and inflammation levels so your body can release the weight it’s been hanging on to. In addition, it makes it easy to make healthier food choices. You didn’t gain those 40 extra pounds in a month, and it will take you time to lose it, but the key is you. You have to draw that line in the sand and start something. 4 months from now, you can be the same weight you are now (or even heavier!), and still have those aches and pains, fatigue, gastrointestinal issues, etc., or 4 months from now you can feel like a million bucks. No one can ever force you to change because the choice truly is yours, but, if you want help and are sincere about making change, I will help you every step of the way!
“LIKE” my page at www.facebook.com/DrJsHealthcare for more information to help you on your weight loss journey!