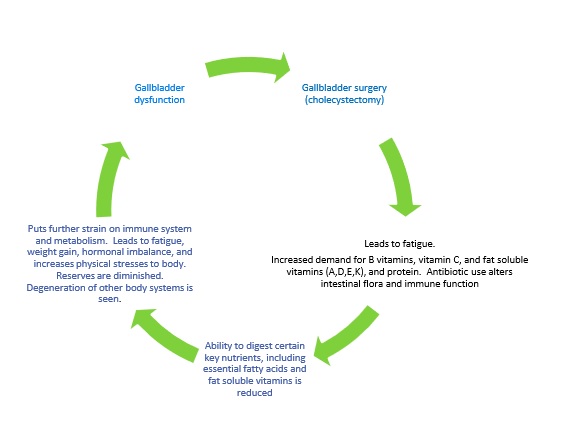
This basic principle applies to any surgery , albeit different organ systems are affected, but for our purposes, we will relate this to gallbladder surgery (cholecystectomy).
ANY time you have surgery (of any sort) you can experience fatigue. Your body only heals when you are asleep – so that is nature’s way of getting you to slow down – so you can heal efficiently [while sleeping]. That said, most people didn’t go into surgery with a fully functioning gallbladder. It could have been dysfunctional or essentially non-functioning for months or even years before that. So , that means you have months or years of digestive issues and not getting the building blocks your body needs to make hormones or repair itself. Surgery brings its own issues, as it increases the demand you have for certain nutrients – like vitamin C, B vitamins, protein, glutathione, etc . So, when you have gallbladder surgery – you go from just being deficient in the fat soluble vitamins (A,D,E,K) and essential fatty acids to being potentially deficient in most of the major vitamin categories. To compound matters, they typically put you on a significant dose of antibiotics after your surgery – which kills off the good bacteria in your gut along with the bad, and since 80% of you immune function comes from the gut and those good bacteria, your immune function goes down , making your MORE tired and susceptible to catching everything that goes around. It is a hard thing to dig yourself out of. You have to overhaul your diet (and you rarely get that advice), you have to get optimal levels of sleep, and you have to get out in the sunshine and fresh air and get some exercise. Otherwise you feel like you are trying to dig yourself out of a hole with a plastic spoon. Now, occasionally people feel great after surgery, but they are the exception to the rule. In 12 years of practice, I have rarely met anyone who didn’t have to make changes to feel better afterwards. Sooner or later their underlying nutritional deficiencies caught up to them and affected their health.
Your body uses cholesterol and vitamin D as precursors to make many of your hormones, including your sex hormones. Fats are necessary for life, and your brain is largely a fatty organ. This is why people taking anti-cholesterol medications (statins) frequently experience decreased libido, or even sexual dysfunction. They also often experience short term memory issues. 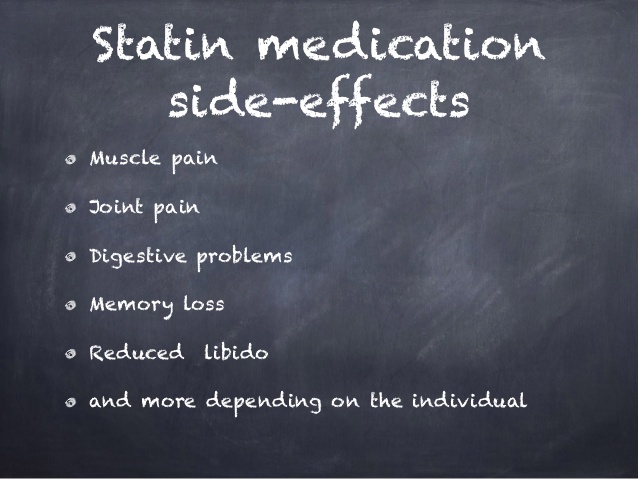
I have heard doctors argue that the gallbladder is unnecessary. They say that since the liver continues to make bile, then fat absorption continues. I disagree with this. First, I don’t believe we were designed with unnecessary parts. We may not realize their full worth or function yet, but that is a human limitation, not a limitation of our creation. Science only ‘discovered’ what the appendix was for within the past few years (It acts as a reservoir for healthy bacteria to recolonize our intestines after fever or illness). Since cholecystectomy is one of the most commonly performed surgical procedures in this country, it makes sense that there is more money in removing them than figuring out how to save them. But I digress, let’s get back to the liver making bile – it does keep making it. The level it makes it is dependent on whether you have fatty liver degeneration or not. But let’s say that you don’t have fatty liver — the liver is going to drip, drip, drip 27-34 oz bile out in a steady stream. That bile is very caustic, and would normally be funneled over to the gallbladder where it is collected and concentrated, up to 18 times – down to 1-3 oz. It is this highly concentrated bile that is designed to break down the fatty acids and fat soluble vitamins you consume. The pre-concentrated bile, while caustic and irritating to your gastric mucosa, can’t hold a candle to the concentrated bile your gallbladder should hold. There is never enough, and never enough at the specific concentration required to absorb those key nutrients out of your diet. So you become deficient and your body goes into conservation mode. Some experience this immediately, others find it takes 6-24 months to fully start experiencing the effects. People find it harder and harder to lose weight, or they find themselves gaining weight despite eating the same diet they always did, or exercising. They find they get fatigued easier, and that they are more susceptible to colds and flu. If they have autoimmune disorders, they may find themselves experiencing a greater degree of symptoms.
So what can you do? I will be the first to admit that I don’t have all of the answers. If anyone suggest that they do – RUN! I can tell you that what my research, and my experience has led me to works for most people. First, you need to keep a food journal and track every meal you eat and how you feel afterwards. Gas, bloating, and diarrhea are the most commonly experienced repercussions from having cholecystectomy. 1 in 15 people who have had their gallbladder removed experience Habba Syndrome, which is commonly misdiagnosed as IBS, or even Celiac Disease. 5-40% of cholecystectomy patients will experience post-cholecystectomy syndrome (persistent right upper quadrant abdominal pain, bloating, gas, nausea, diarrhea, and general malaise). Often, these people will know the whereabouts of every bathroom in their vicinity, because they experience issues almost immediately after eating. Dietary changes will be necessary. Certain foods aggravate a significant number of people with no gallbladder. These include greasy foods, carbonated beverages, dairy, and simple carbohydrates. Wheat products, including breads and beer, can also elicit a negative response. Please don’t take this as a reason to stop eating healthy fats — you NEED to consume them in order to maintain your health and shift your waistline. Use specific dietary supplementation to replace some of the action of the gallbladder. I recommend a blend of ox bile, beet concentrate and pancrelipase to substitute for this action. If you avoid fats, you will make matters worse. Since digestive enzyme production decreases with age, if you are over 40, adding digestive enzymes to your meals can also cause significant relief. make sure you are getting adequate levels of sleep so that your body can repair itself and so that levels of stress hormones can decrease.
- Keep a food journal to log your physical responses to foods and beverages. Learn what your body can and cannot handle.
- Use specific dietary supplements to increase your digestion and resolve your underlying nutritional deficiencies.
- Get 7+ hours of uninterrupted sleep per night.
- Get out there and move. Aerobic activity and weight bearing exercise is crucial for your recovery. Walking is a great way to get started. Walking in the sunshine is even better (get some vitamin D while you are at it!)


Wish I could have read this before my surgery. What a hoax on the people having them subject to this madness.. I never feel well and cannot lose weight.
My name is Ronny and my doctor insisted that I should schedule to have my gallbladder removed because I have been experiencing discomfort in the upper abdominal area for some time now. I have had 2 sonograms done and both scans came out inconclusive of anything wrong I also had a hyida scan with the nuclear injection to track things in my body and nothing wrong could be found, the reason why my doctor suggested having the surgery of a cholecystectomy (removal of the gallbladder) is because my insurance is running out and I would not be covered in the near future and that my body can function with out a gallbladder and such. Well I am having second thought’s and have already decided to opt out of the surgery and get more of a understanding of what is wrong with myself and find out all the alternatives rather the do something IMO seems drastic and have surgery based on a factor of not having insurance, I am not in extreme pain and can function for the most part normally , hell I went to work today ( I work in construction) I still do have discomfort and some pain at times and other times I do not at all, it likes comes and goes sparatacally, I know I am up there in age I just turned 50 and Both my parents and my sisters have had this surgery, my brother did not though and we look a lot alike though there is ten years in age between us. I do know that I weigh more now then I ever did in the past @ 210 pounds I am 6’1”, I used to be on average 185 pounds, and I am concerned that it may be my diet and over weightiness contributing to this problem I am experiencing. I like to get peoples opinions on this and what they think. Thank you for reading and leaving a response.
Before I had my gallbladder removed, I was having severe stomach pain. I visited a doctor who told me that my body was poisoned, and gallbladder removal was inevitable. After surgery, I felt terrific right away, and remained that way for quite sometime. Then my triglyceride count went through the roof, so much so, that a proper cholesterol count couldn’t be done.
I was then told that my body has lost a certain enzyme, and that for the rest of my life I would have to take fenofibrates. My tryglyceride count fell from 13 to 8 and a second cholesterol test was performed. My cholesterol was measured at 11 at its worst thus far. I was then prescribed crestor which I refuse to take. I now am gaining weight constantly and am forever tired. My strength has diminished and breathing is laboring if I do anything strenuous. I just don’t know what to do at this point, my doctor has no clarifying answers, I have a constant stitch feeling in my left side, what can I do?
Hello Ronny,
My upper abdominal pains started out as sporadic as well. In time, they grew stronger and longer. There were times I couldn’t help but cry, I thought I was dying. After several doctor visits, I learned that my body was poisoning itself due to issues with my gallbladder. I was even tested for Hepatitis C. Infection was spreading throughout my body. Blood counts were through the roof. All because I left it for too long. The surgeon immediately admitted me and removed my gallbladder. It was instant relief, everything went back to normal. Though you must diet properly and exercise after on a regular basis or weight gain becomes a problem. Though we need our gallbladder for the breakdown of fats in the stomach, you can live a good life without one.
I had a very flat stomach before I had my gallbladder removed. I was 97 lbs. Now I have belly fat! My gallbladder looked fine (that is what the doctor said after taking it out!) The doctors said that the sonar gram looked like I had a stone but when they removed, there were no stones!
I went in with a fever and pain on my right side. My pulse was rapid and my blood pressure was low. I never told the doctor I had pain on my right side. It only hurt on the left. I later discovered it my have just been a pancreatic issue. He just wanted to make money! I am so upset and never feel or look like I used to. This has been 5 years now and it is just getting worst.
i have many of the symptoms of a bad gallbladder, but am reluctant to go for surgery, or even visit the doctor?
is there medication i could take, or is removal the only option?
I would definitely get it looked at, my doctors did not believe it was my gallbladder because my pain was more located in my back, turns out it was setting farther back than a normal gallbladder and I had a 10.2mm gallstone stuck in my bile duct and it was causing my liver to start failing, it can be quite dangerous if it is a gallbladder issue that progresses too far,
Where can I get the supplements ox bile, beet concentrate and pancrelipase? My surgeon suggested papya tablets and does this help with digestion after surgery should I take this for the rest of my life after/before every meal
You can click on the ‘SHOP’ tab on my website and order directly.
So,
I had my first gall bladder attack. First I’ll explain what I was doing wrong and how it happened. I used to drink a lot. Recently I quit, as I’m 25 and trying to settle down. So on the weekend I decided I would drink after being clean for a while. As per usual it was a binge drink, so the next morning I was nursing a hangover. Of course, a normal young adult eats greasy food to feel better. But after a few hours I was in agony.
I just thought of it as nothing, “I’ve been eating healthy for a month, exercising and counting calories, my body just can’t handle the drinking and greasy food” so I tried sleeping it off. I woke up crying, never have I felt that pain. I knew it was my stomache, but after the crazy pain I wound up in the hospital. Nice, a hamburger sent me to the hospital. Fat people can eat 30, I eat one and immediately my body hates me. So they do he urinalysis, blood tests and ultra sound. I had gallstones, small gall stones.
The doctor immediately said “I’ll schedule emergency surgery for you to have it removed” thank God my boyfriend was like “no, I have insurance, I’m looking for a good surgeon who won’t leave scars” so we left. The doctor then explained if I remove the stones they will only come back bigger…. and it needs to be done immediately.
Since they are small, I started googling. Haven’t stopped. I’ve been on every website, every thread and contacted many people/doctors.
I found a way to naturally get rid of them, and am now on my second day of eating a lot of apples. The acid in apples softens them, and when they’re soft enough you take laxatives along with high fatty foods and high acidity. Apparently they come out painlessly.
Now I’m just terrified of what will happen, if you gets blocked it’ll be emergency surgery. I’m even so embarassed to tell my friends, and only close relatives know.
My stupidity. I drink, yo-yo diet, lose more than 10 pounds within a month and yo-yo back. Native American desent. Female. Limit calories and fat. Limit foods. 500 calorie a day binders. Never drank juice. Only drank water.
There was so many ways to prevent it and so many symptoms I had for years. The main symptom is an itchy stomach lining after eating eggs, which happens to 95% of people with gallstones. No, stupid me wrote it off as an allergy.
If only I knew of this before. If only I had a fighting chance to prevent it. We’re all in the same boat. We all fit into many categories.
Uhh. If I do this an one gets lodged. I’m unsure of what to do at the moment.
Either way I’ll be fat, lazy with thin hair. Do I try and maintain or get rid of????
Be very cautious about partaking in any gallbladder ‘cleanses’. They can cause far more harm than good. If you read my other GB posts, there are some that address what to do if you still have stones, or your GB function is depressed.
I know it happens to most people, I just never thought it would happen to me, you know?
I had my gallbladder removed just a little over a year now, I wish I had known then what I’m finding out now as I’m in ten times worse shape then having a gallbladder that did contain small stones but, this was found on accident I’d asked my doctor if we could order an US because I was bloating to the point I looked 6 or 7 mos. pregnant I need to add I’m a medical Assistant and work in the clinic my pcp is at anyway I had been having low back pain in my L-spine area which I chalked up to me recently exercising again and not being 20 something anymore but, 39 I’m now 40 after the US RUQ pain so bad I was in tears was referred to general surgeon whom of course said the gallbladder needed to come out I should of known better I should have done research because I’m so worse off now I can’t eat anything good for you or bad for you without the urgent need to run to the bathroom for a year now nothing but, diaherra several times daily I get nauseous even vomit I’m always tired my body is inflamed I still have pain RUQ under my ribs I’ve gained weight rapidly I’m taking 40 pounds heavier than when I had the surgery I still get extremely bloated it’s effected my job as I’ve missed several days from illnesses to just plain exhaustion I never would have done this surgery if I’d of known all of this along with my blood work being all over the place from having elevated liver enzymes I.e I don’t drink to my thyroid dipping into Graves’ disease looking results only to have tests redone and all returns to normal except my WBC it’s been elevated for a long time though as far back as 2013 but, I’m sure whatever else might be wrong with me medically none of this post gallbladder removal is helping. My boss even said I’ve not been the same since having that surgery. I have some things to work on with my diet I know this so after reading all the great information provided Dr. Miranda I’m going to focus on getting my body out of starvation mode. The real kicker to this is I knew all it was due loosing my gallbladder your body knows and it tells your subconscious which then tells your conscious and it eats at you in the back of your mind causing you to hunt down and validate what your thinking and feeling even what I’ve said out loud I really need to get some relief from this calm it down I also have gerd worse than ever before I have to take otc omeprazole daily my cholesterol is horrible Trigs are off the charts in 600 range.